
Vascular imaging techniques used to diagnose carotid stenosis have advanced considerably in recent years, especially ultrasound imaging. Recall that benefits are less marked in cases of moderate stenosis (50%–70%) and marginal in cases of asymptomatic stenosis. 4 Although surgery may be beneficial for patients with symptomatic stenosis of 50% to 70% or asymptomatic stenosis, surgical treatment – whether endarterectomy or angioplasty with/without stenting – must be considered on a case-by-case basis. Risk levels were higher for stenosis exceeding 90% (35% of all vascular events/year) than for stenosis in the 70% to 79% range or stenosis >99% (yearly risk of 11%).
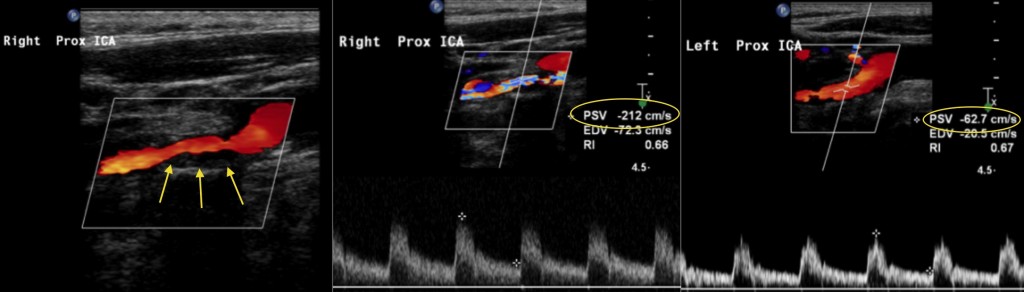
The recurrence rate was only 7.2% in patients who also underwent surgical treatment. 4,5 In cases of stenosis ≥70%, 24.4% of patients receiving medical treatment experienced recurrence during a 2-year follow up period. The procedure was assigned a recommendation level of A since it decreased overall risk of new cerebrovascular events by about 50% compared to a group receiving medical treatment only. The NASCET 3,4 and ECST 5 studies showed that under certain conditions, carotid endarterectomy effectively prevented stroke recurrence in patients with symptomatic stenosis ≥70% who had experienced TIA or mild cerebrovascular event. 2 The degree of stenosis of the internal carotid artery (ICA) is the most important indicator of risk of stroke, and the basis on which doctors decide if endarterectomy is needed. The risk of recurrence is particularly high in strokes with an atherothrombotic mechanism. 1 With this in mind, identifying and treating arterial stenosis correctly is a top priority. 1 TIA precedes a disabling infarct in up to 43% of patients with a stroke of atherothrombotic origin. It is estimated that 28% of ischaemic strokes occurring in Spain are atherothrombotic in origin, and that most are caused by carotid stenosis. Se revisan los hallazgos que permiten cuantificar el grado de estenosis carotídea extracraneal utilizando tanto el estudio ultrasonográfico carotídeo como el transcraneal, con un especial énfasis en la importancia de la valoración de signos indirectos.
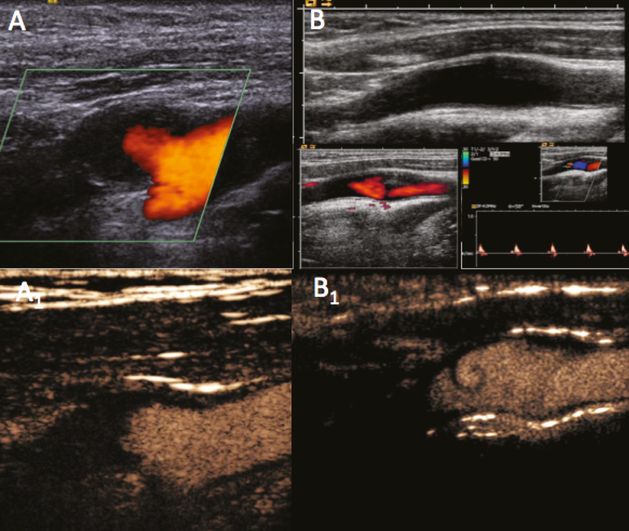
En esta revisión se detalla la metodología para la evaluación de la estenosis carotídea desde el punto de vista ultrasonográfico, siguiendo las recomendaciones de consenso establecidas por la Sociedad Española de Neurosonología (SONES). Las alteraciones de la velocidad de flujo en el punto de máxima estenosis junto con los cambios hemodinámicos en regiones proximales (arteria carótida común) y distales (carótida interna postestenótica, arteria oftálmica y polígono de Willis) permiten cuantificar con precisión la estenosis carotídea. La ultrasonografía es la técnica más habitual para el diagnóstico de la estenosis carotídea.


 0 kommentar(er)
0 kommentar(er)
